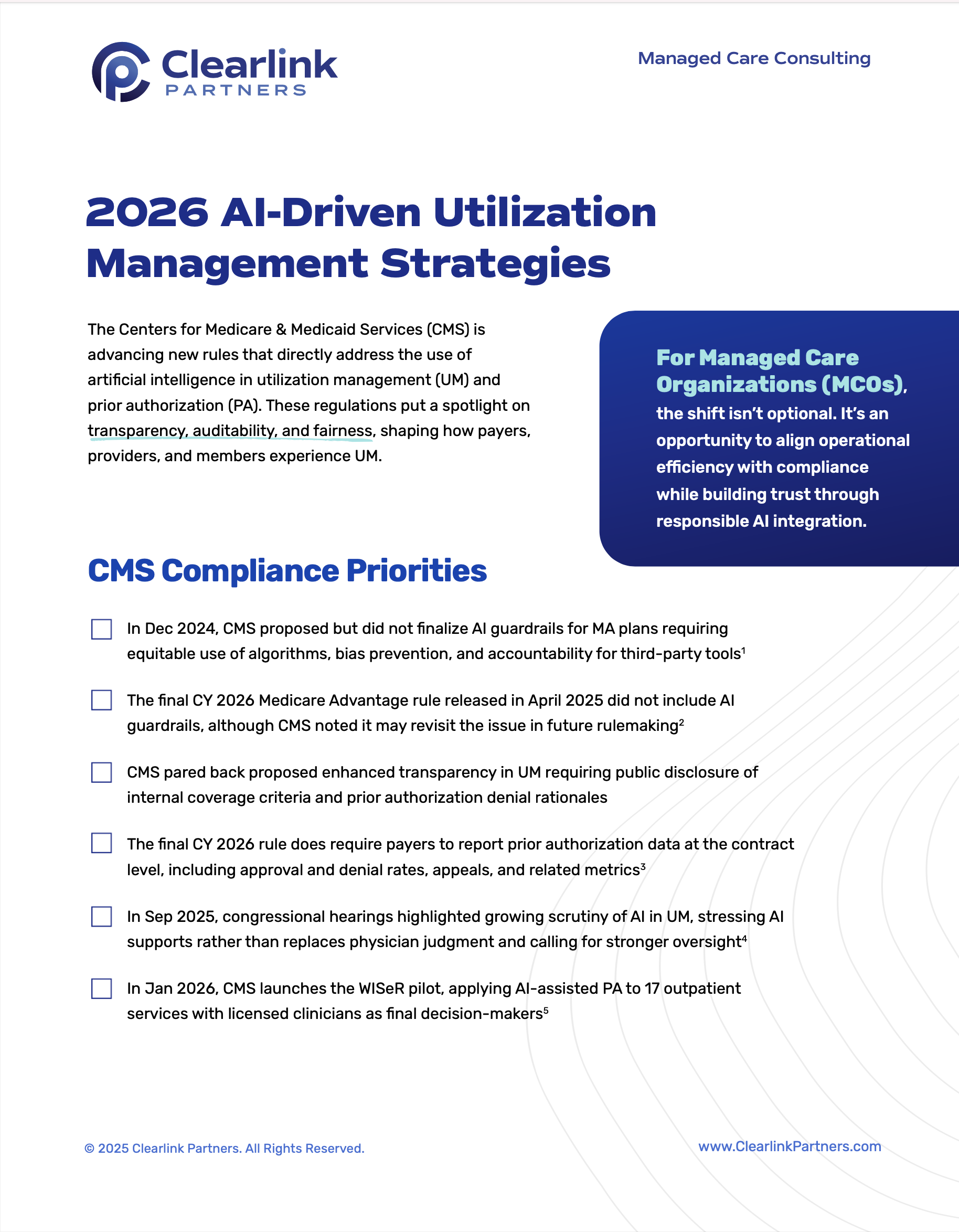
The Centers for Medicare & Medicaid Services is advancing new rules that directly address the use of artificial intelligence in utilization management and prior authorization. These regulations put a spotlight on transparency, auditability, and fairness, shaping how payers, providers, and members experience UM. For managed care organizations, this is an opportunity to align operational efficiency with compliance while building trust through responsible AI integration.
Learn more by requesting the free tip sheet.