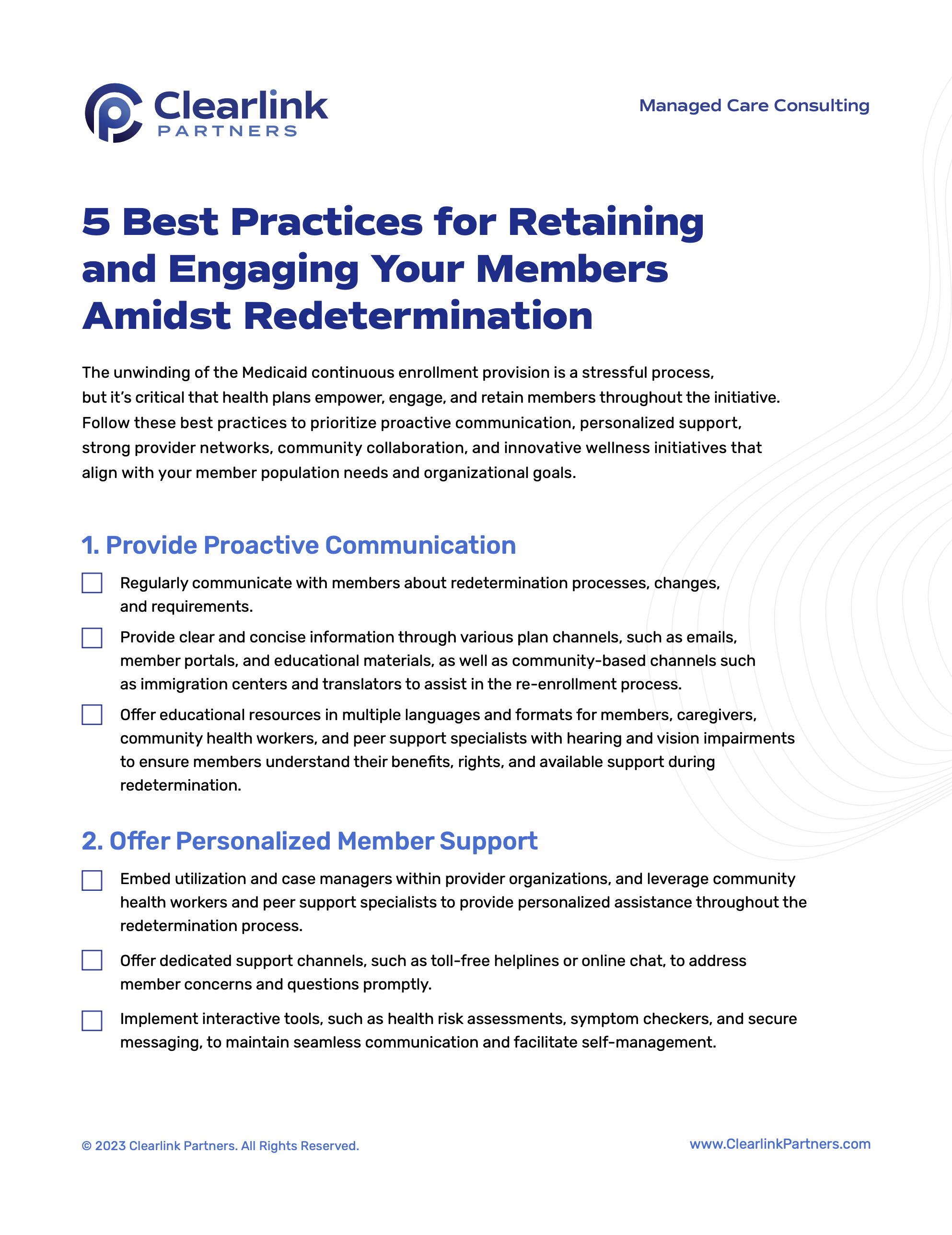
The unwinding of the Medicaid continuous enrollment provision is a stressful and complex process, but it’s critical that health plans empower, engage, and retain members throughout the initiative. Organizations can follow several best practices to prioritize proactive communication, personalized support, strong provider networks, community collaboration, and innovative wellness initiatives that align with member population needs and organizational goals. Get tips for maximizing member satisfaction and elevating your product continuum in the face of redetermination using a free tip sheet from Clearlink.
Learn more by requesting the tip sheet.