Authors: Karin VanZant, Vice President, Social Determinants of Health & Health Equity & Linda Uwumarogie, NCQA Accreditation Manager
The National Committee for Quality Assurance (NCQA) is a non-profit organization dedicated to improving healthcare quality. Its tagline, “We work for better health care, better choices, and better health,” reflects its commitment to enhancing healthcare outcomes—and its significant impact means that 73% of insured Americans are now covered in NCQA-accredited plans.1
NCQA offers health quality recognition products for health plans, providers, other healthcare entities, and data and technology resources. Among its most recognized products is Health Plan Accreditation (HPA), a highly sought-after recognition across government, commercial, and exchange health insurance programs, with over 173 million people enrolled in an accredited health plan throughout the country.2 HPA is now required in 3 out of 4 states.
Source: https://reportcards.ncqa.org/
In 2010, NCQA added a Distinction in Multicultural Health Care (MHC) program based on the Office of Minority Health’s Culturally and Linguistically Appropriate Services (CLAS) Standards.3 The MHC distinction provided assurances that health plans had increased awareness, policies, and processes in place to meet these standards, fostering a broader and deeper understanding of equity in their culture.
What is NCQA’s Health Equity Accreditation?
In 2021, NCQA announced a pilot program to test two new accreditation products called Health Equity Accreditation (HEA) and Health Equity Accreditation Plus (HEA Plus), available as a three-year status for a broad range of healthcare organizations. The standard HEA product focuses on gathering demographics to examine member needs and determining opportunities for reducing disparities and enhancing the cultural and linguistic appropriateness of care.1
The HEA Plus is an advancement of the HEA that involves more robust data collection and partnering with community-based organizations and others to address members’ social needs and mitigate community social risks.1 Nine healthcare organizations, including plans and hospital systems, participated in the pilot, which launched in December 2021, offering feedback on both HEA accreditation standards. In July 2022, NCQA officially replaced the MHC with the Health Equity Accreditation programs.4 These programs—and others, such as LTSS Accreditation and PCMH Recognition—aim to help plans integrate equity into all quality offerings as NCQA believes quality care is equitable care, and there is no quality without equity.1
With the introduction of these new accreditation programs, organizations across various healthcare sectors have begun pursuing HEA to enhance their approach to equitable care.
Which Organizations are Eligible for HEA?
In the dynamic landscape of healthcare, various organizations are pursuing HEA, each playing a unique role in fostering inclusivity and accessible care. The following types of organizations may apply for HEA:
- Health plans
- Managed behavioral healthcare organizations
- Organizations that provide disease management, population health, case management, or wellness services
- Clinically integrated organizations (e.g., accountable care organizations)
- Hospitals/hospital systems
- Medical centers
- Primary and specialty care practices, clinics, and Federally Qualified Health Centers
What are the Benefits of HEA or HEA Plus Status?
HEA acknowledges organizations that focus on health equity work and foster an internal culture to support their external activities. Research shows that health disparities not only limit health outcomes but are burdensome, resulting in excess costs and decreased productivity.5 The HEA establishes language services and provider networks that meet members’ cultural and linguistic needs, identifies opportunities to reduce health disparities, and improves whole-person care. With HEA, organizations actively build and integrate equity into their policies and practices to improve health outcomes and reduce disparities. NCQA also seeks to integrate health equity into Healthcare Effectiveness Data and Information Set (HEDIS) results by stratifying HEDIS measures by race and ethnicity, incorporating new measures to address unmet social needs, and making HEDIS more inclusive of gender identity.1
NCQA cites several key reasons why organizations should achieve and maintain HEA or HEA Plus status:1
- Improving quality and equity for members by empowering your team to identify and act on health disparities
- Creating the structure and accountability to achieve and sustain health equity quality improvement objectives
- Demonstrating to regulators, members, and others that improving health equity is more than a trend in healthcare
- Anticipating and aligning with the requirements of state and federal regulations across care models, contracts, and payment programs
- Educating your team and showcasing your expertise in improving services, care, and member health
HEA products have specific standards that healthcare organizations must meet, some of which are derived from the standards in the MHC Distinction.6 While several have been slightly updated, some are entirely new.
NCQA’s Health Equity Accreditation Standards
To achieve Health Equity Accreditation, organizations must meet a set of structured requirements designed to enhance healthcare access, reduce disparities, and promote culturally competent care. These standards ensure that organizations have the necessary policies, processes, and infrastructure in place to provide equitable services.
The seven key HEA standards include:
- Organizational Readiness
- Race/Ethnicity, Language, Gender Identity & Sexual Orientation Data
- Access & Availability of Language Services
- Practitioner Network Responsiveness
- Culturally & Linguistically Appropriate Services Programs
- Reducing Health Care Disparities
- Delegation of Health Equity Activities
NCQA’s Health Equity Accreditation Plus Standards
For organizations that want to go beyond the foundational accreditation, HEA Plus introduces additional requirements that focus on data integration, cross-sector collaboration, and addressing social risk factors at the community level.
The four additional HEA Plus standards include:
- Collection, Acquisition & Analysis of Community & Individual Data
- Cross-Sector Partnerships & Engagement
- Data Management & Interoperability
- Program to Mitigate Social Risks & Address Social Needs Referrals, Outcomes & Impact
How to Prepare for Health Equity Accreditation
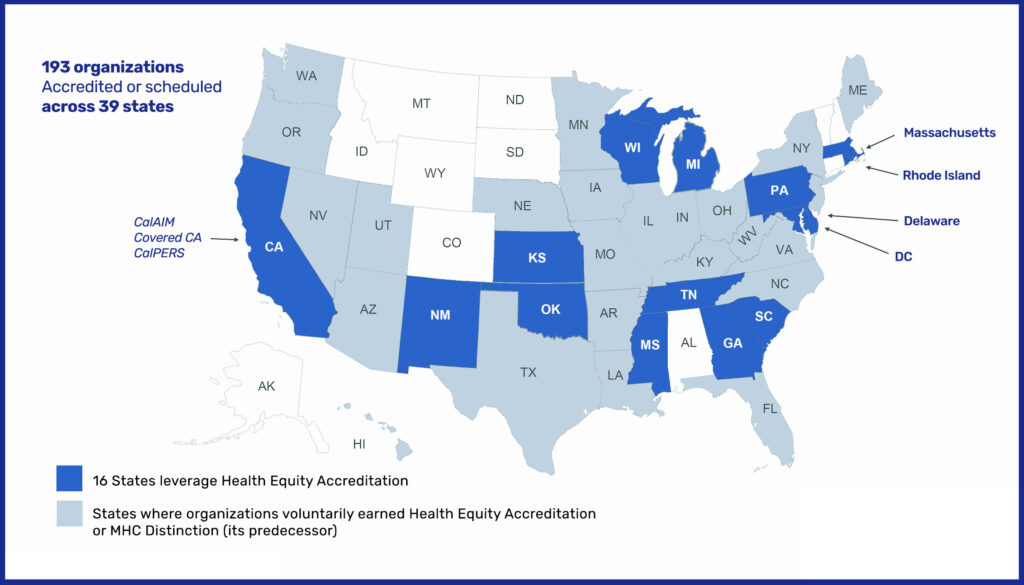
As of March 2023, 61 health plans had achieved their HEA, with additional plans on track to complete their NCQA surveys throughout the year.7 By October 2023, NCQA reported that 193 organizations across 39 states were either accredited or had scheduled their accreditation.1
Plans should also consider CMS’s recently released Inpatient Prospective Payment System (IPPS) Final Rule for CY2023, which includes two new equity-focused measures called SDOH-01 and SDOH-02 and requires hospitals to attest to whether they are prioritizing equitable care. Plans can anticipate that CMS may release similar requirements in the future, as CMS has a history of using its regulatory authority to promote health equity.
Health plans should take immediate action to integrate health equity into their policies and procedures, encouraging collaboration with community groups, government agencies, and key stakeholders. The benefits of acting on this now go beyond collaboration:
- Prepare for competitive bids in states that will require it for procurements.
- Streamline the accreditation process by integrating HEA standards early.
- Enhance recruitment efforts by demonstrating a commitment to Diversity, Equity, and Inclusion (DEI).
- Improve quality measurement and reduce health disparities across your patient populations.
Preparing for Health Equity Accreditation with Clearlink
Clearlink is working with health plans to assess the next steps, conduct gap analyses, review policies and procedures, and guide our clients who are considering transitioning from the MHC distinction to HEA within their next review period. Clearlink offers a Readiness Assessment Tool to help organizations assess where they need to strengthen their policies and processes to prepare for the HEA and secure their survey date. Clearlink’s team of industry leaders and consultants work with clients to assist them in being best prepared for these new requirements, integrating health equity into your existing operational framework, and future-proofing for health equity accreditation.
Several states are embedding this new accreditation into contract renewals and procurement processes. Managing a new accreditation in addition to RFP procurements and contractual implementation processes can be challenging for your staff, especially during a busy year with Medicaid redeterminations and new quality requirements.
Health equity is not only a matter of social responsibility, but it is also a critical component of providing high-quality healthcare. Plans have a vital role to play in ensuring equitable access to care for their members. By seeking NCQA HEA, plans can improve healthcare outcomes, increase member satisfaction, enhance care delivery, and contribute to building healthier communities. Don’t wait to get started on the path to achieving HEA accreditation. Schedule a meeting with us today.
Sources:
- NCQA, “Health Equity Programs for Health Plans”
- NCQA, “Health Plan Accreditation”
- U.S. Department of Health and Human Services, “National CLAS Standards”
- NCQA, “NCQA’s Health Equity Accreditation Programs”
- Kaiser Family Foundation, “Disparities in Health and Health Care: 5 Key Questions and Answers”
- NCQA, “Proposed Standards Updates for Health Equity Accreditation 2023”
- Becker’s Payer, “Every plan awarded NCQA’s health equity standard, state-by-state”
- NCQA Health Equity Accreditation Eligibility Reference Guide, NCQA 2022
